1
Improve Existing Systems
Ending mistreatment of women during childbirth
INTRODUCTION
In Zambia, behaviorally informed solutions designed by ideas42 have led to more respectful maternity care, including better pain management during labor and delivery. This can also make it more likely that women will give birth in facilities, providing a safer experience for both mothers and infants than at-home births.

CHALLENGE
A third of women experience disrespect and abuse while giving birth in health facilities.
This is a global problem: studies in countries of all income levels have found that a high proportion of women are subject to scolding, insults, and other harsh treatment from care providers during delivery. In addition to eroding the quality of the birth experience, disrespect and abuse can have longer-term negative health impacts as women can become discouraged from seeking postnatal care and may opt to have subsequent births away from health facilities, without support from skilled providers. Additionally, because women share what they’ve been through with peers, a negative experience can dissuade even more women from giving birth in a facility even though it’s ultimately safer.


In many facilities, mistreatment has become normalized, so staff don’t face severe consequences for abusive behavior.
When new members join the maternity care team, they soon see that their peers often speak harshly in urging clients to follow instructions. Influenced by these workplace norms, as well as their own life experiences (they may have received similar treatment themselves), new staff conclude that such behavior is acceptable. They see that when other staff members direct unkind words or actions toward a mother, it’s rationalized as being for her own good. And those who may disapprove, including supervisors, colleagues, and clients who are upset at how they’re being treated, have no clear way to take remedial action and stop the behavior.
Mistreatment of women during childbirth is closely linked to the management of their pain.
Midwives and other caregivers, understandably guided by their training and ongoing supervision, tend to focus almost exclusively on the infant’s and mother’s survival. They view the pain of childbirth as secondary—and inevitable—and therefore they have limited strategies to alleviate it.


Birth care providers don’t see that a woman’s failure to follow their instructions may in fact be exacerbated by her experience of pain.
Nor do they appreciate that abusive treatment tends to make a mother cower or withdraw, so she may not inform them when she is having problems during birth.
Providers are also unaware of the negative impact that disrespectful care can have on both immediate and long-term health outcomes.
They receive no feedback or follow-up reports showing how harsh treatment can lead to difficulties during delivery and may also affect a woman’s future choices around seeking care for herself, her child or future births.

The context birth care providers work in, where their number one priority is avoiding the death of the baby or mother, leads many to feel that their decisions are reasonable.
To end abusive treatment and reduce pain during childbirth, therefore, step one is to change that context.
RESPONSE
For ideas42 and our partners, creating the conditions for more respectful maternity care starts with systematic, behaviorally informed design.
In 2018, we found the ideal opportunity to apply our expertise—through a collaboration among birthing women, care providers, health administrators, and policymakers in Zambia. Our team worked with the organization Safe Motherhood 360+ as part of the Breakthrough RESEARCH portfolio funded by USAID.
Together, we leveraged our formative research to develop four solutions that reduced abusive treatment, improved pain management, and fostered greater empathy among care providers. We then launched a pilot study in partnership with Zambia’s national Ministry of Health and the District Health Office of Chipata, in the eastern part of the country.

SOLUTIONS
1
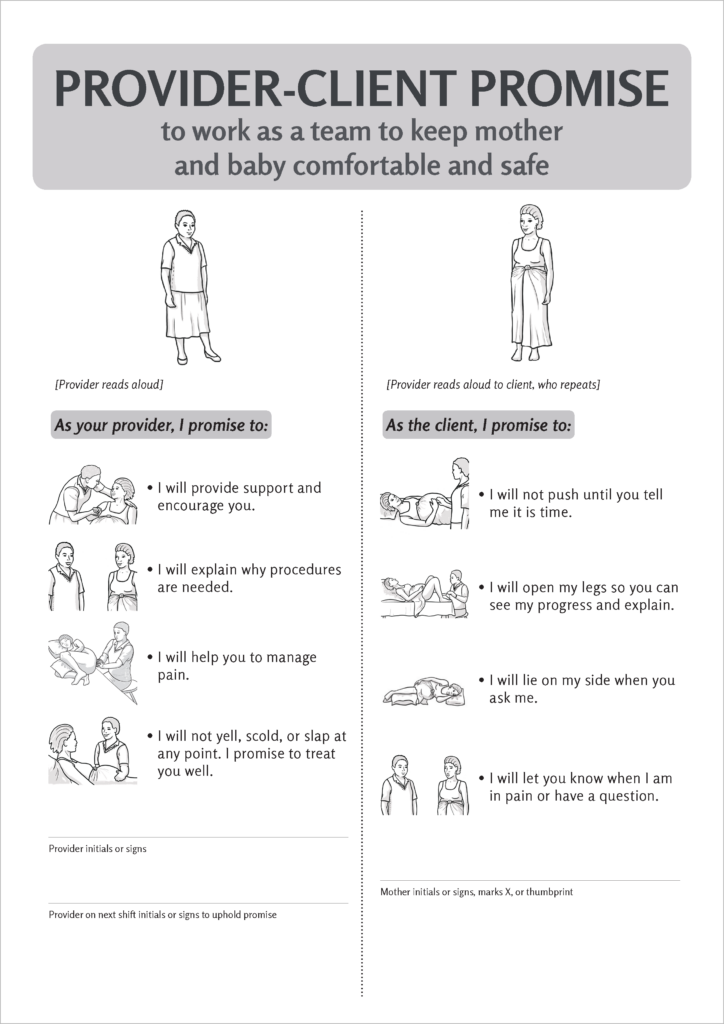
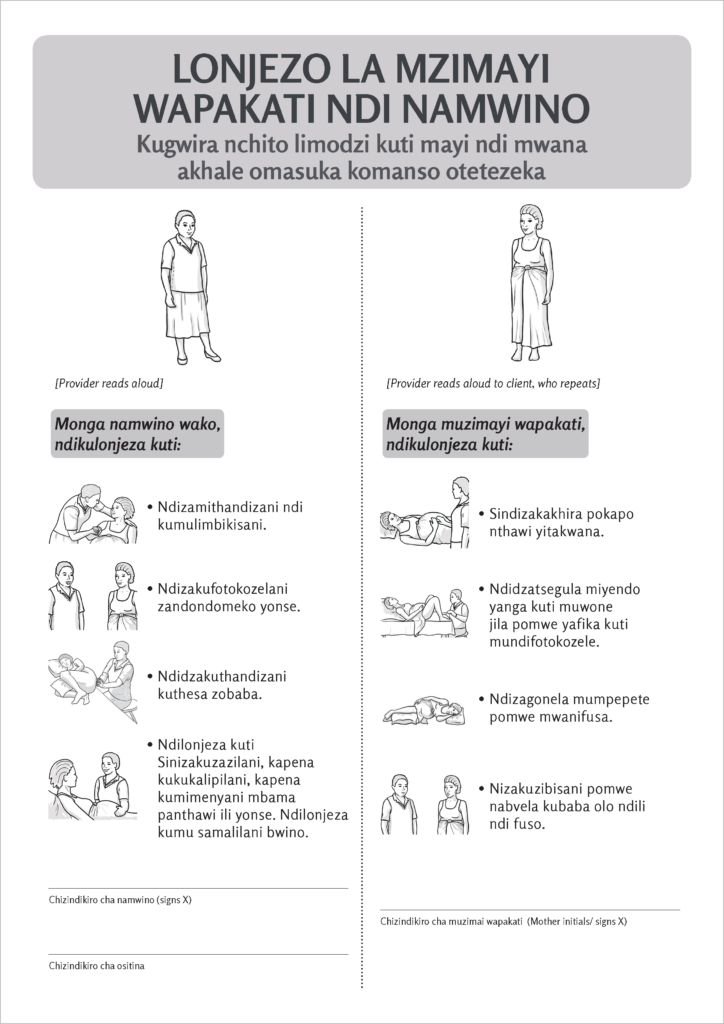
Provider-Client Promise
- This formal pledge between provider and client begins by reinforcing a fundamental point: the expectant mother is an equal partner in the childbirth process. On being admitted to the health facility to give birth, the mother discusses with the midwife and other care providers—and then confirms in written or spoken words—their shared commitment to a positive, respectful relationship.
- Providers spell out exactly what the mother should expect and what in turn is expected of her. This helps neutralize the most frequent trigger of disrespectful care: providers’ perception that a client is refusing to comply with requests or guidance, when in fact she doesn’t fully understand them.
- Most importantly, providers commit not to yell, scold or abuse the mother.
- The promise aims to create a balanced power dynamic between provider and client, establishing a safe space defined by common objectives and grounded in trust.
2
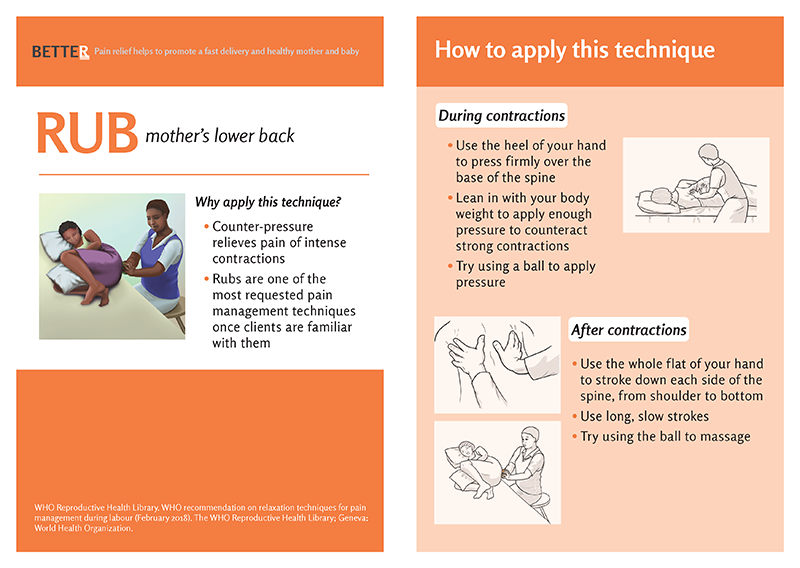
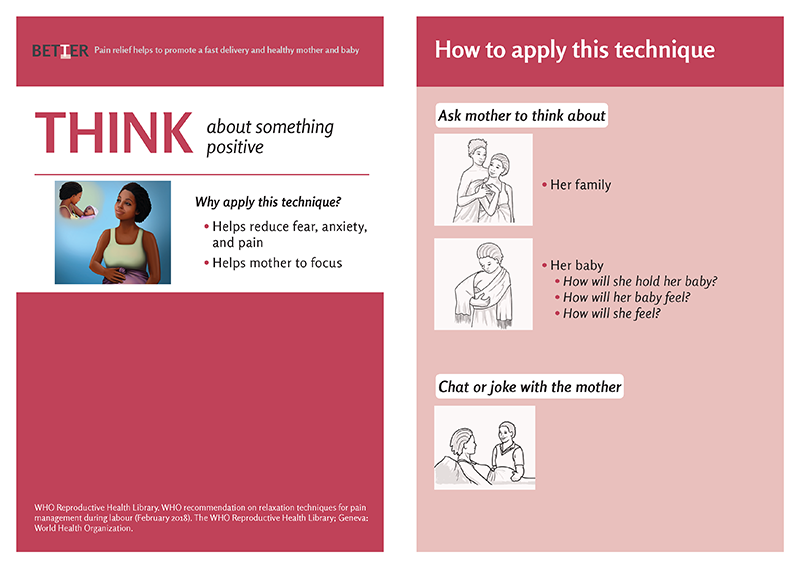
Pain Management Toolkit
- The toolkit is designed to reinforce the central importance of (nonmedicated) pain management during childbirth. Pain is not the price a mother must pay while providers address more important concerns; helping her successfully manage pain is a pillar of responsive, holistic clinical care.
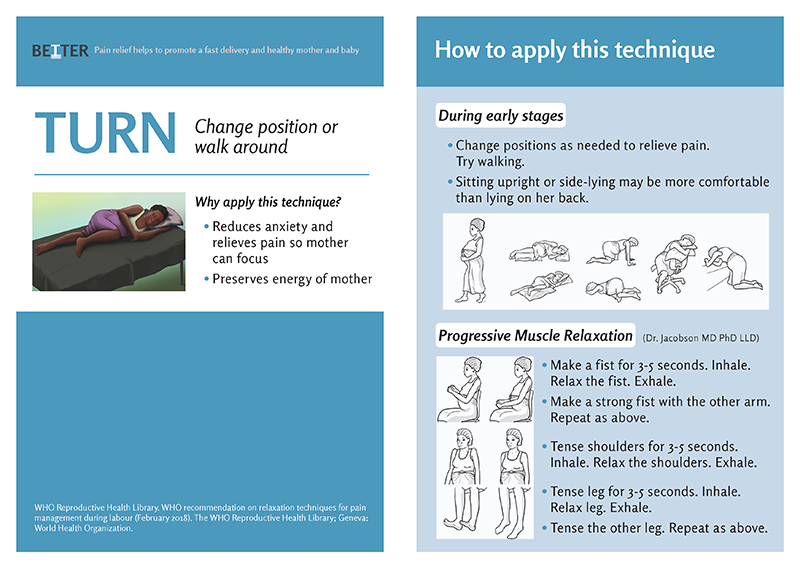
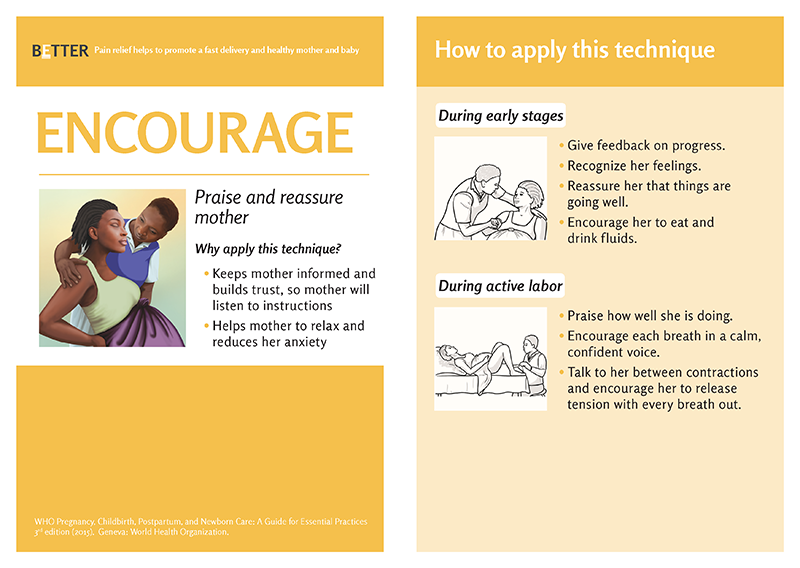
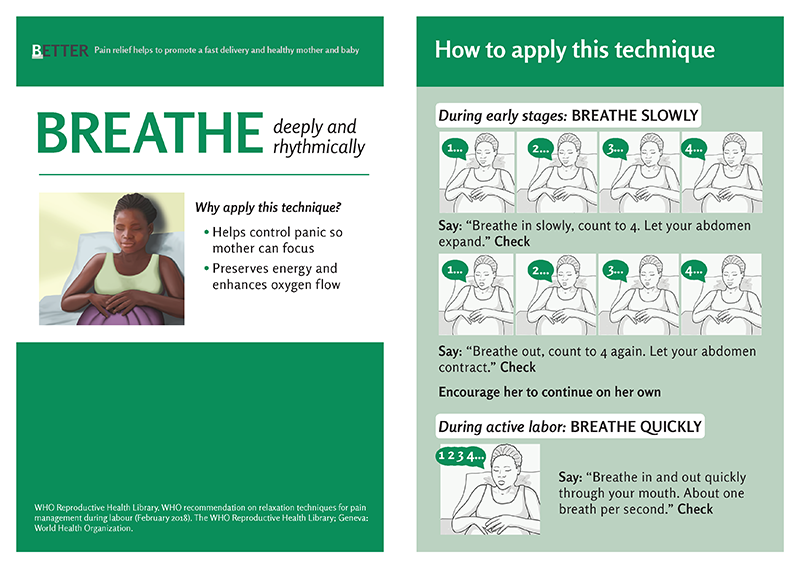
- The kit comprises a manual explaining pain management using the BETTER model (Breathe, Encourage, Turn, Think, Rub); a poster reinforcing the BETTER techniques with visual cues; and a partograph that incorporates pain management into the routine monitoring and recording of data as labor progresses.
- The pain management toolkit sets the expectation that clients should ask for and receive support from their providers. At the same time, it reminds providers to guide mothers in managing their pain throughout delivery. And it helps mothers focus on providers’ encouragement and prompts, reducing the risk of harm to the baby while helping relieve the tensions that can lead to abuse and disrespectful care.
3
Client Feedback Box
- Suggestion boxes are a widely offered but typically underused device for soliciting feedback on maternity care. Placed far from the labor ward, they tend to be inconvenient for clients, who are exhausted from giving birth and reluctant to venture elsewhere in the facility. Also, the need for pen and paper makes it even more difficult to provide suggestions. And for the many clients with literacy challenges, written feedback is simply not a feasible channel.
- Direct feedback from clients, however, is vital to ensuring that staff focus on quality of service—especially in an area as sensitive as childbirth. So the ideas42 team, leveraging behavioral insights from our formative research, set out to design a better mechanism for collecting clients’ views on their experience with maternity care.
- As a first step, the new client feedback box is conveniently located in a health facility’s labor and delivery area—but in a place where it’s generally not visible to care providers.
- Instead of written comments, the feedback box employs simple tokens that clients drop through labeled slots corresponding to satisfaction levels.
- Providing feedback is easy; every mother receives a token that she can deposit when she is discharged. While traditional suggestion boxes mainly capture comments from only the happiest or most dissatisfied clients, the feedback box attracts responses from a more representative array of clients. This includes many who might have hesitated to report a negative assessment, whether from fear of reprisals or because they feel their experience may not have been bad enough to warrant lodging a complaint.
- For care providers, meanwhile, the feedback box reinforces the importance of evaluating clients’ experience and provides a focus for discussions about improving performance. Going forward, measuring progress is a simple matter of comparing the tallies of tokens for each rating level.
4
Reflection Workshop
- The final piece in this package of behavioral design solutions is a facilitated workshop in which care providers share ideas and best practices, explore potential changes in their approach, and set goals for further improving mothers’ childbirth experience.
- The workshop uses context-setting games and role playing to spark reflection and foster deeper empathy among providers.
- The overarching message is that respectful care should be seen not as exceptional, but as routine maternity care. The workshop sessions guide participants to new ways of evaluating their interactions with clients and—even more important—committing to specific actions that will drive positive change.
RESULTS

15%
Abusive care reduced by 15 percentage points
In a 2019 trial, the pilot’s 10 sites showed a decrease of 15 percentage points in reported instances of disrespectful treatment during childbirth, compared with the experience of mothers at other health facilities in the Chipata region. This positive result shows the value of continuing to use such low-cost interventions to steadily improve care.
Increased pain- management support
Women at pilot sites made more frequent requests for help in handling childbirth pain, and providers placed greater emphasis on pain management as part of routine care.
IMPACT
Results of the pilot were shared with health professionals at an event co-hosted by Safe Motherhood 360+ and Zambia’s Ministry of Health. Ministry officials undertook to incorporate the behavioral solutions into a national policy aimed at fostering more respectful maternity care.


The results are replicable and scalable. We’ve already begun adapting the ideas42 approach for use in Liberia through the Breakthrough ACTION project funded by USAID.
These simple, low-cost behavioral interventions can help advance maternity care globally. We’re confident that the solutions developed in Zambia and adapted in Liberia can be adapted and implemented in other contexts as well. Based on the successes to date, we believe this work will inspire care providers and entire health systems to ensure that all women going through childbirth are free from abusive treatment and have more support in managing their pain.